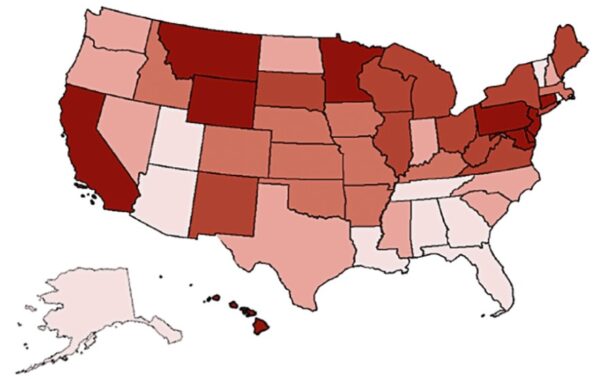
The impact of Covid-19 on hospitals in the U.S. has created historic financial challenges for most facilities, according to a study conducted by the American Hospital Association (AHA). With the recent uptick in cases nationwide, particularly in the Southern states, ERs and ICUs are filling up again and facilities are beginning to see more cancellations and postponements of non-emergent procedures. Demand for medical equipment and supplies is also increasing, driving up costs to treat hospitalized patients suffering from the virus.
Simultaneously, high unemployment rates have caused a sudden rise in the number of uninsured patients that hospitals are seeing and admitting. The number of uninsured could hit as much as 40 million should unemployment rates continue to rise. Loss of insurance puts families at financial risk and has already caused an increase in uncompensated care for U.S. healthcare providers. U.S. hospitals reported charity and bad debt write-off increases totaling 13% in March 2020 over March 2019.
Hollis Cobb Revenue Cycle Solutions Helping Providers Weather the Covid Impact
Hollis Cobb provides a wide range of services to health systems nationwide from front-end to back-end. Company leadership has been creative during the Covid crisis, assisting providers in finding innovative ways to generate revenue while providing quality care to patients in need.
In addition to early out and bad debt collections, services include:
- Insurance follow up
- Pre-Service Collections
- Pre-Auth/Pre-Reg
- Payment Monitoring
- Denials resolution
- Customer Service
- Scheduling
- Credit Balance resolution
- A/R work-down
- Custom revenue cycle projects
As hospital revenue cycle staff have transitioned to remote work environments, the Hollis Cobb team has been available to step in and fill any gaps for our clients to help them keep billing and collection productivity at the highest levels possible during this pandemic.
Financial Impact in Numbers
The AHA analyzed the financial impact of Covid-19 on healthcare providers between March 1 and June 30, 2020. In this four-month timeframe, the AHA estimates that U.S. hospitals have faced combined losses totaling $202.6 billion or an average of $50.7 billion per month. Along with increased Covid admissions and postponed non-emergent services, additional purchases of personal protective equipment (PPE) along with overtime pay and childcare provided to hospital staff have all contributed to these unprecedented financial losses over a short period of time.
The Centers for Disease Control and Prevention (CDC) estimates an overall hospitalization rate of 29.2 per 100,000 people due to the surge in hospital and ICU admissions. The rates increase according to patient age to 47.2 per 100,000 for patients aged 50-65 and 95.5 per 100,000 for patients over 65. The average cost for treating a Covid patient is $20,000 according to the Kaiser Family Foundation, and $88,000 for patients requiring the use of a ventilator.
Facing Revenue Challenges
Prior to the Covid-19 pandemic, many U.S. hospitals were already facing financial pressures brought on by low reimbursement rates from government and commercial payers. The unexpected pandemic added fuel to the fire pushing some healthcare facilities toward negative margins. Financial support provided by Congress has served to stabilize providers so that their doors can remain open during this healthcare crisis; however it has not restored hospital revenues to pre-Covid levels.
The first half of 2020, hospitals nationwide have seen an average decline of 13% in patient discharges resulting in significant loss of revenue while costs have increased. This decrease is primarily due to the postponement of non-emergent procedures along with patients choosing to cancel primary and specialty care physician visits. Patients who are neglecting chronic disease care for fear of Covid exposure stand to further jeopardize their health resulting in higher healthcare costs.
What Health Systems Can Do to Recover from the Financial Impact of Covid-19
According to information compiled by the Healthcare Financial Management Association, there are steps healthcare systems can take to regain their financial footing now and as the U.S. emerges from the pandemic.
- Establish a leadership position responsible for coordinating and communicating a recovery plan.
- Determine what recovery numbers should look like, and set targets and goals for achieving those numbers.
- Communicate to the entire organization expectations and methods for achieving established goals.
- Stress quality over quantity in recovery efforts to avoid a decline in the patient experience.
- Track results and provide data and guidance daily to each revenue cycle team.
- Engage with business partners and outsourcing firms where possible to reduce costs.
Health Systems that begin developing a recovery plan now, while the pandemic is still in full force, will be better prepared to implement the plan once Covid admissions start to decline again.